Age-related macular degeneration (AMD)

What is age-related macular degeneration?
Age-related macular degeneration (AMD or ARMD) is an eye condition affecting central vision. It causes blurry vision and other visual symptoms that may be gradual or sudden. In adults aged 50 and over, macular degeneration is a top cause of irreversible vision loss.
AMD affects the macula — the small round area in the center of the retina — which is located in the back of the eye. The macula plays a crucial role in your vision. It maintains your sharpest central vision, allowing you to see fine details when you look directly at something.
The health of the macula helps determine your ability to see color and perform detailed visual tasks, such as:
See and read written text
Recognize faces
Drive a car
Watch television
Use a digital device
A person with AMD eye disease loses central vision but maintains peripheral (or side) vision. It can occur in one or both eyes and may affect each eye differently.
As a progressive condition, AMD tends to worsen over time. However, blindness is rare in age-related macular degeneration.
SEE RELATED: Visual impairment: What is impaired vision?
Types of age-related macular degeneration: Dry vs. wet
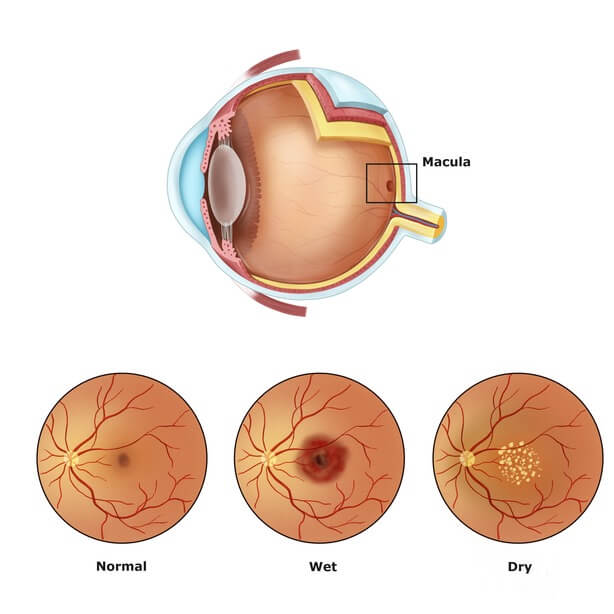
Click on image to enlarge.
There are two types of age-related macular degeneration: dry AMD and wet AMD. Each variation of this degenerative eye disease carries unique characteristics.
Characteristics of dry AMD
Dry AMD (also called non-exudative or atrophic AMD) is the most common form of macular degeneration, affecting 80%-90% of AMD patients. It is called “dry” macular degeneration since it does not involve blood vessel leakage, as seen in the wet form. (Dry AMD is not the same as dry eye, which is a different type of eye condition.)
Age-related macular degeneration typically begins as dry AMD.
Dry macular degeneration involves the gradual thinning and breakdown of the macula. It is associated with yellow-colored deposits beneath the macula called drusen. These deposits are accumulations of proteins and fatty substances. (The presence of drusen does not always indicate macular degeneration. However, having a higher amount of drusen can lead to the development of AMD eye disease.)
Most individuals with dry macular degeneration notice a gradual loss of vision that progresses with time. People with dry AMD can develop wet AMD.
Central vision loss tends to occur more slowly with dry macular degeneration.
Characteristics of wet AMD
Wet AMD (also called exudative or neovascular AMD) is the more visually threatening form of the condition. It accounts for 10%-20% of AMD cases. Wet AMD is responsible for 80%-90% of severe cases of vision loss resulting from age-related macular degeneration.
Wet macular degeneration is caused by leaky blood vessels in the retina. New or abnormal blood vessels may develop and leak fluids or blood into the back of the eye, damaging the macula. In wet AMD, this growth of new blood vessels is called choroidal neovascularization.
People with wet AMD typically experience more significant central vision loss than those with dry macular degeneration.
Wet macular degeneration can have a sudden onset. Vision loss tends to occur more quickly with this type of AMD and can even develop over the course of a few days to several weeks.
Signs and symptoms of age-related macular degeneration
The symptoms of macular degeneration can vary according to the disease stage. They can also differ from one person to the next. In many cases, individuals with AMD disease do not notice signs or symptoms of the condition until it has progressed. Pain is generally not an AMD symptom.
Early warning signs
The early stage of AMD disease generally does not cause any symptoms. Rather, symptoms of macular degeneration typically develop in the intermediate stage.
Macular degeneration symptoms often involve signs of vision loss and may include:
Dark or shadowy areas in your central vision
Blind spots in your field of vision (scotoma)
Unusually blurry, fuzzy, wavy or distorted near vision
Difficulty seeing details in poor lighting conditions
Changes in color vision
Progression of symptoms
Many patients do not notice the symptoms of AMD disease if they are present in only one eye. This may also be the case if symptoms are more pronounced in one eye than the other.
Seeing wavy or distorted words when reading is often a sign of late-stage AMD.
Stages of AMD
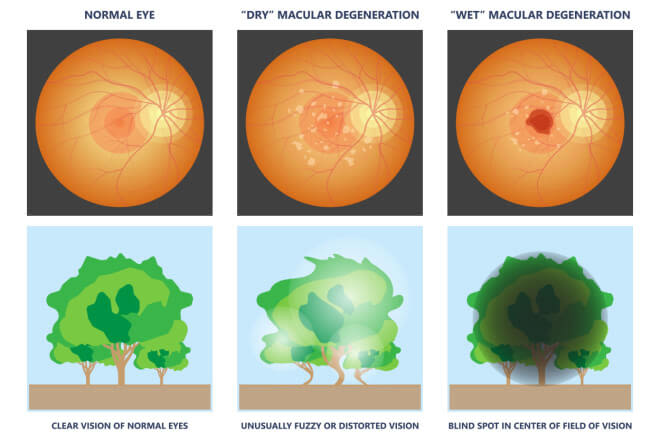
Click image to view how the different types of macular degeneration may present.
There are three stages of dry macular degeneration:
Early – The initial stage of AMD eye disease typically causes no symptoms or vision loss.
Intermediate – When the disease advances to the intermediate stage, blurry areas may develop in your central field of vision.
Advanced – During the late stage of dry macular degeneration, you may experience blurry, missing or wavy areas in the center of your vision. This may gradually lead to a total loss of central vision.
Dry macular degeneration can develop into wet AMD at any of these disease stages. When wet macular degeneration develops, however, it is considered to be in the advanced stage of the condition. Wet AMD is faster progressing and almost always begins as dry macular degeneration.
In some instances, dry or wet AMD may only affect one eye. Macular degeneration may also progress differently in each eye. This means that each eye may experience different stages of the disease.
What causes age-related macular degeneration: Who is at risk of AMD?
While the precise cause of AMD eye disease is unknown, it is believed that a range of factors may contribute to its development. Vision concerns caused by this degenerative eye disease can vary among individuals.
Macular degeneration can affect anyone. However, certain factors can increase the risk of developing the condition. These include:
Age
As its name implies, age-related macular degeneration becomes more of a risk with age. The severity of vision loss from the condition also tends to increase over time. Those over age 50 have a greater chance of developing AMD.
Around 30% of adults over the age of 75 have age-related macular degeneration.
Genetic factors
Macular degeneration is associated with aging and other factors, but there also may be a genetic component. Researchers have noted strong associations between AMD and two gene variants.
Having a genetic predisposition to AMD does not mean you will automatically develop it. However, it can increase your risk of experiencing the disease.
If one of your parents has AMD, your chances of getting the condition are nearly twice as high as someone without a genetic predisposition.
Sex
Macular degeneration affects more women than men. This may be due to women having a longer life expectancy than men.
AMD eye disease is associated with inflammation in the body. Women could be at a higher risk for macular degeneration given the different inflammatory responses that occur in men and women. Women tend to have higher levels of inflammation than men, which can also contribute to depression. (AMD can increase the risk of developing mental health issues such as depression.)
Women tend to experience the onset of AMD eye disease at a younger age than men.
Ethnicity
Among U.S. adults, AMD is most prevalent in the white population. Individuals of white (non-Hispanic) ethnicity have a higher likelihood of developing the disease when compared to other racial groups.
Health factors
Specific health issues have been linked to AMD eye disease and may increase a person’s risk of having the condition. These health concerns include:
Cardiovascular disease (heart disease) – Some cardiovascular diseases can damage the blood vessels of the eyes. This may contribute to macular degeneration.
Hypertension (high blood pressure) – High blood pressure may also play a role in the development of eye conditions, including macular degeneration.
Inflammation and immune response – Some research studies show that inflammation, and the body’s response to it, increase the risk of AMD.
Obesity – People who are overweight or obese are at a higher risk of developing AMD eye disease. Those with a higher body mass index (a score of 30 and above) may be more than twice as likely to get the condition.
Environmental and lifestyle factors
Certain environmental and lifestyle factors may increase the risk of AMD, including:
Smoking – Smoking cigarettes can quadruple a person’s chances of developing AMD. It is a major risk factor for this eye condition.
Sedative lifestyle – Inadequate amounts of exercise can affect heart health and potentially increase the risk of AMD eye disease.
Diet – Eating a diet that is high in saturated fat, cholesterol and foods like white bread and pasta can contribute to obesity. It may increase the risk of age-related macular degeneration.
Ultraviolet (UV) light – People with a history of more UV light exposure may be at a higher risk for macular degeneration, as UV light is thought to damage the retina. Some researchers believe that over-exposure to sunlight also may be a contributing factor in the development of the disease. However, this theory has not been proven conclusively.
The risk factors consistently found in studies to be associated with AMD are aging and smoking.
How is AMD diagnosed?
The early stage of dry macular degeneration generally does not cause noticeable symptoms. Even some cases of intermediate dry AMD may not produce symptoms. To catch AMD eye disease as soon as possible, it is important to see an eye doctor at least once a year for a comprehensive eye exam.
An ophthalmologist or optometrist may use one or more of the following techniques to detect macular degeneration:
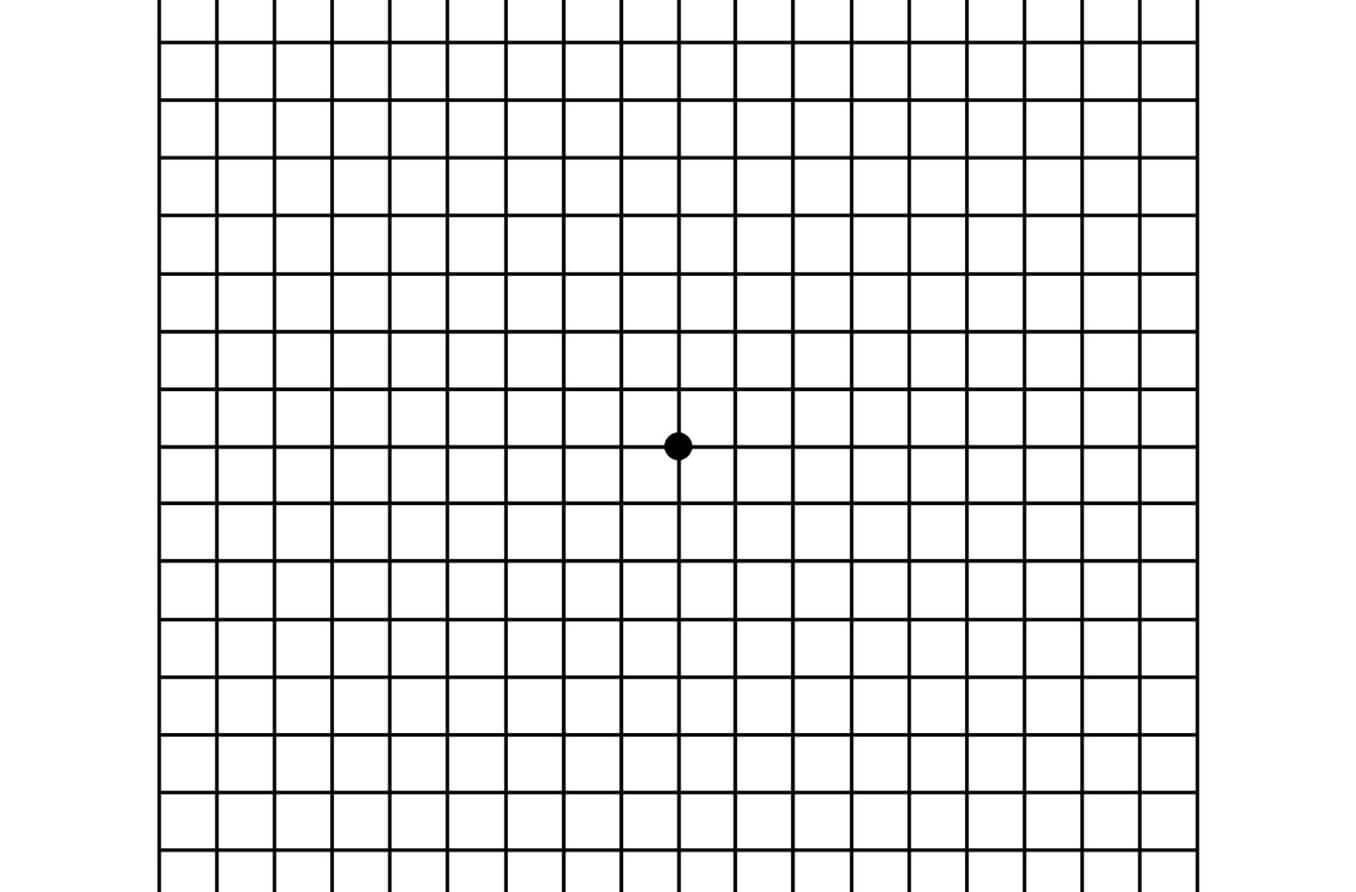
Visual acuity test – A visual acuity test is commonly given during routine eye exams. It is used to measure the strength of a person’s vision at various distances. It may also incorporate the Amsler grid to test their ability to see straight lines.
Dilated eye exam – A dilated eye exam involves special drops that widen the pupils so an eye doctor can get a clearer view of the retina.
Fluorescein angiography – With this technique, a special dye called fluorescein is injected into the arm. As the dye travels through the bloodstream, images are taken of the eye to see if any blood vessel leaks are present under the macula.
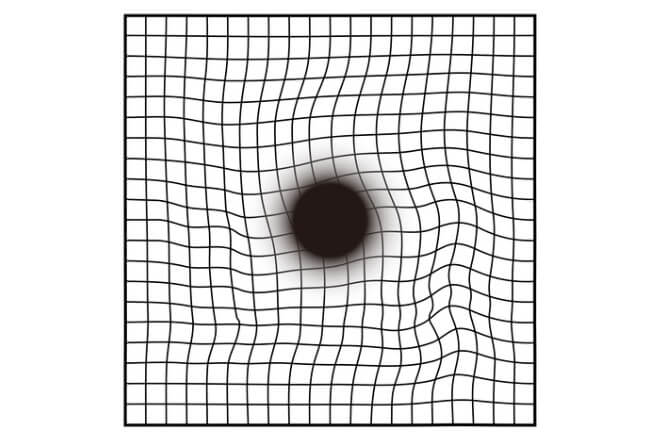
Amsler Grid: someone with macular degeneration may see some of the lines as wavy or blurred, with some dark areas at the center.
Fundus autofluorescence imaging – When parts of the retina are exposed to specific wavelengths of light, they naturally light up (or fluoresce). Eye specialists can use the results of this imaging to monitor the health of the retina and the progression of macular degeneration.
Optical coherence tomography (OCT) or optical coherence tomography angiography (OCTA) – The OCT device takes images of the back of the eye as you look into the machine. OCTA differs slightly in that it uses laser light reflection as well as the OCT device to show how blood flows through the vessels in the eye.
AMD treatments
While there is no cure for macular degeneration, vision impairment and the severity of symptoms may be decreased with early diagnosis and treatment. Some treatments may slow, delay or prevent its progression. Certain AMD treatments may also improve or stabilize a person’s vision.
Treatments for macular degeneration depend on whether the disease is in its earlier-stage dry form or the more advanced wet form. Treatment may also vary according to individual needs and other factors.
Treatment for dry AMD
Two medications are FDA-approved to treat an advanced form of dry AMD known as geographic atrophy (GA). Syfovre (pegcetacoplan) and Izervay (avacincaptad pegol) are injectable treatments administered directly into the eye.
Treatment options for early-stage dry macular degeneration are limited at this time. Taking certain vitamins and minerals may help reduce the risk of dry macular degeneration progressing to wet AMD. A research study known as the Age-Related Eye Disease Study 2 (AREDS2) found that a specific formulation of supplements may help lower the risk of advanced AMD by 25%.
The AREDS2 formulation includes:
Vitamin C
Vitamin E
Lutein
Zeaxanthin
Copper
Zinc
An eye care specialist can determine if nutritional supplements might be beneficial for you.
Treatment for wet AMD
For wet AMD, the goal of most treatments is to shrink or stop abnormal blood vessel growth and prevent the leakage of fluid into the retina. Wet macular degeneration treatments may include:
Anti-vascular endothelial growth factor (VEGF) injections – The most common treatment for wet AMD is the injection of a medication (such as Avastin, Lucentis, Eylea or Beovu) into the affected eye. These injections, known as anti-VEGF injections, help control the leakage and abnormal growth of blood vessels in the back of the eye.
Laser photocoagulation – Another technique that is performed for wet AMD is laser photocoagulation. This treatment uses an intense light beam to seal leaking blood vessels.
Photodynamic therapy – This treatment may be used in certain cases of wet AMD. It combines laser technology and a special medication that is injected into the arm. After the injection, an eye doctor will administer anesthetic eye drops and focus the laser onto the eye. When exposed to the laser’s light, the medicine creates blood clots in the abnormal macular blood vessels to seal them off.
The implantable miniature telescope (IMT) is an additional treatment option for some patients with end-stage AMD. Surgically placed in the eye, this device helps improve a person’s vision by enlarging the images they see.
Other methods of treating wet and dry macular degeneration are currently under investigation.
Low vision aids
For AMD patients who have suffered any degree of vision loss, low vision devices — such as magnifiers, telescopes and apps on digital devices — can help maximize their vision potential. Large-print products may also be available for further accessibility. Low vision aids contribute to quality-of-life improvements for people with long-term vision loss.
Complications of AMD
The main complication of age-related macular degeneration is central vision loss. Central vision gradually decreases, leaving only side (peripheral) vision. This can make normal activities like reading, driving and distinguishing images difficult. People with severe or late-stage AMD eye disease could be considered legally blind.
AMD may also lead to other eye-related complications. These include:
Subretinal hemorrhage (bleeding in or around the macula)
Vitreous hemorrhage (blood in the vitreous humor)
Exudative retinal detachment (the retina becomes detached due to leaking blood vessels)
Diplopia (double vision)
It is thought that up to 50% of individuals with macular degeneration experience Charles Bonnet syndrome. This condition involves visual hallucinations that are specifically associated with vision loss.
Other complications that can arise from AMD are mental health issues, including depression and anxiety. Macular degeneration causes vision loss, which affects a person’s ability to function as they used to. As such, this visual impairment can increase the risk of experiencing mental health conditions.
Further complications include the increased risk of accidents and the inability to drive.
When to see an eye doctor
If you notice sudden or gradual changes in your central vision, see your eye doctor to rule out macular degeneration as the cause. Yearly comprehensive eye exams are recommended as preventative care. They can also help identify conditions like macular degeneration as early as possible.
Regular eye exams are also essential for monitoring the health of AMD eyes and detecting any vision changes.
Eye care specialists can identify early signs of macular degeneration before symptoms develop. Your eye doctor will likely dilate your eyes to evaluate the retina/macula. They may use imaging tools to observe any retinal changes.
Your eye doctor can also answer questions or address concerns you have about AMD’s effect on your eye health. Questions asked by patients with AMD eye disease may include:
What is macular degeneration?
What is AMD eye disease?
What are the symptoms of macular degeneration?
What causes macular degeneration?
Is macular degeneration progressive?
How is AMD treated?
If you have vision loss or other macular degeneration symptoms and are already seeing an AMD specialist, schedule an exam with an eye care practitioner specializing in low vision rehabilitation. These vision care specialists can evaluate your vision and your daily needs to maximize function.
Prevention of AMD
Gaining an awareness of AMD and understanding your personal risk factors may be the first step in preventing the condition. Maintaining a healthy lifestyle, such as getting regular exercise, eating a balanced diet and avoiding tobacco use, might help inhibit its development.
Comprehensive eye exams also play an important role in AMD prevention and reducing the risk of permanent vision loss. Find an eye doctor near you to schedule a comprehensive eye exam and learn more about macular degeneration.
READ NEXT: Maculopathy: Causes, symptoms, types and treatments
What is macular degeneration? American Academy of Ophthalmology. EyeSmart. November 2023.
Age-related macular degeneration. American Academy of Ophthalmology. EyeWiki. August 2023.
Macular degeneration. American Optometric Association. Accessed November 2023.
View how macular degeneration may affect vision. BrightFocus Foundation. November 2021.
Macula. Cleveland Clinic. May 2022.
Macular degeneration. Cleveland Clinic. February 2023.
Age-related macular degeneration (AMD). National Eye Institute. June 2021.
Age-related macular degeneration (AMD). Johns Hopkins Medicine. Accessed November 2023.
Age-related macular degeneration (AMD or ARMD). Merck Manual Professional Version. April 2022.
MicroRNAs as diagnostic and prognostic biomarkers of age-related macular degeneration: Advances and limitations. Neural Regeneration Research. March 2021.
Symptoms of wet age-related macular degeneration (AMD). BrightFocus Foundation. August 2021.
Soft drusen may indicate early macular degeneration. UCLA Health. June 2022.
New treatments for age-related macular degeneration. American Academy of Ophthalmology. EyeSmart. February 2023.
What to know after a macular degeneration diagnosis. American Academy of Ophthalmology. EyeSmart. March 2023.
Symptoms of wet age-related macular degeneration (AMD). BrightFocus Foundation. August 2021.
Macular degeneration: Essential Facts. BrightFocus Foundation. July 2023.
Age-related macular degeneration: Facts & figures. BrightFocus Foundation. March 2023.
Macular degeneration: Frequently asked questions. BrightFocus Foundation. July 2023.
Genetics and age-related macular degeneration. American Academy of Ophthalmology. EyeSmart. January 2023.
Age-related macular degeneration. MedlinePlus [Internet]. October 2021.
Macular degeneration: Prevention & risk factors. BrightFocus Foundation. October 2021.
Is macular degeneration hereditary? BrightFocus Foundation. January 2023.
Gender difference in ocular diseases, risk factors and management with specific reference to role of sex steroid hormones. Journal of Mid-life Health. January-March 2022.
The roles of sex and gender in women’s eye health disparities in the United States. Biology of Sex Differences. October 2021.
The role of inflammation in age-related macular degeneration: Updates and possible therapeutic approaches. Asia-Pacific Journal of Ophthalmology. March-April 2023.
Sex differences in markers of oxidation and inflammation. Implications for ageing. Mechanisms of Ageing and Development. April 2023.
The role of inflammation in depression and fatigue. Frontiers in Immunology. July 2019.
Prevalence of age-related macular degeneration (AMD). Division of Diabetes Translation, National Center for Chronic Disease Prevention and Health Promotion. CDC. October 2022.
Association between age-related macular degeneration and risk of heart failure: A population-based nested case-control study. Journal of the American Heart Association. July 2021.
Blinding eye disease linked with forms of cardiovascular disease. Ophthalmology Times. November 2022.
Lower your risk of macular degeneration. American Academy of Ophthalmology. EyeSmart. January 2021.
How smoking can contribute to vision loss and blindness. U.S. Food & Drug Administration. April 2022.
UV radiation linked with early AMD onset. Review of Optometry. September 2023.
Risk factors for progression of age-related macular degeneration. Ophthalmic and Physiological Optics. February 2020.
Visual acuity test. Cleveland Clinic. November 2022.
Macular degeneration diagnosis. Stanford Medicine. Accessed December 2023.
Get a dilated eye exam. National Eye Institute. May 2021.
Fundus autofluorescence. American Academy of Ophthalmology. EyeWiki. September 2023.
An update on fundus autofluorescence. Review of Ophthalmology. September 2023.
FDA approves new treatment for geographic atrophy. American Journal of Managed Care. August 2023.
A new era in dry AMD treatment. Duke Ophthalmology. Duke University School of Medicine. February 2023.
Vitamins for AMD. American Academy of Ophthalmology. EyeSmart. November 2023.
Treating difficult cases of wet AMD. Review of Ophthalmology. March 2023.
Treatments for wet AMD (advanced neovascular AMD). National Eye Institute. June 2021.
How effective are age-related macular degeneration treatments? BrightFocus Foundation. November 2022.
Injections to treat eye conditions. National Eye Institute. July 2022.
Laser photocoagulation for age-related macular degeneration. Johns Hopkins Medicine. Accessed November 2023.
Photodynamic therapy for age-related macular degeneration. Johns Hopkins Medicine. Accessed November 2023.
Implantable miniature telescope (IMT). Kellogg Eye Center. University of Michigan Health. Accessed December 2023.
Low vision aids. StatPearls [Internet]. August 2023.
Types and causes of retinal detachment. National Eye Institute. December 2020.
Subretinal hemorrhage. The Eyes Have It. University of Michigan Kellogg Eye Center Department of Ophthalmology and Visual Sciences. Accessed December 2023.
Vitreous hemorrhage. StatPearls [Internet]. August 2023.
Diplopia (double vision). Cleveland Clinic. December 2021.
Charles Bonnet syndrome: A condition of the visually impaired. Annals of Eye Science. September 2022.
Macular degeneration diagnosis. BrightFocus Foundation. Accessed December 2023.
Low-vision therapy for macular degeneration: How it can help. BrightFocus Foundation. August 2021.
Learn about age-related macular degeneration. Division of Diabetes Translation, National Center for Chronic Disease Prevention and Health Promotion. CDC. November 2020.
Prevention of the onset of age-related macular degeneration. Journal of Clinical Medicine. July 2021.
Page published on Friday, March 1, 2019
Page updated on Tuesday, February 20, 2024
Medically reviewed on Sunday, February 4, 2024